This study guide provides comprehensive preparation for sterile processing technicians, covering essential topics like infection control, sterilization methods, and quality assurance to ensure exam success and professional competency.
1.1 Overview of the Role and Responsibilities
A sterile processing technician ensures medical instruments are properly cleaned, sterilized, and prepared for surgical procedures. Key responsibilities include decontamination, packaging, sterilization, and storage of equipment. Technicians must adhere to strict infection control protocols and maintain accurate documentation. Strong attention to detail and teamwork are crucial, as their work directly impacts patient safety and surgical outcomes. This role is vital in maintaining aseptic environments and ensuring operational efficiency in healthcare settings.
1.2 Importance of Certification in Sterile Processing
Certification in sterile processing validates a technician’s knowledge and skills, ensuring adherence to industry standards and patient safety. It demonstrates expertise in infection control, sterilization techniques, and quality assurance. Certification enhances career opportunities and is often required by employers. Organizations like HSPA promote certification, emphasizing its role in maintaining high professional standards and public trust in healthcare settings. It is a critical step for career advancement and professional credibility.
1.3 Key Concepts Covered in the Study Guide
This study guide covers essential topics such as infection control, sterilization techniques, and quality assurance. It includes detailed chapters on preparation and packaging, sterilization methods, and regulatory compliance. Key concepts like decontamination, biological safety, and waste management are also emphasized. The guide prepares technicians for certification exams and real-world challenges, ensuring a solid foundation in sterile processing best practices and adherence to industry standards.

Preparation and Packaging for Sterilization
This section details proper instrument preparation, cleaning, and inspection methods. It also covers packaging materials and techniques to ensure items are sterilized effectively and remain sterile post-process.
2.1 Principles of Proper Instrument Preparation
Proper instrument preparation involves thorough cleaning, inspection for damage, and functional testing. Instruments must be disassembled, lubricated, and organized to ensure efficient sterilization. This step prevents contamination and ensures all surfaces are exposed for effective sterilization, maintaining patient safety and instrument longevity. Adherence to these principles is crucial for achieving optimal sterilization outcomes and maintaining the integrity of medical instruments.
2.2 Packaging Materials and Methods
Packaging materials like wraps, containers, and pouches ensure instruments remain sterile until use. Double wrapping or using impervious materials prevents contamination. Packaging must allow steam or chemical penetration while maintaining sterility. Proper sealing and labeling are critical. Instruments are arranged to prevent damage and ensure even sterilization. Aseptic presentation post-sterilization ensures patient safety and adherence to infection control standards.
2.3 Importance of Labeling and Documentation
Accurate labeling and documentation ensure traceability of sterilized items, confirming they meet safety and quality standards. Proper labels identify contents, sterilization methods, and dates, while documentation tracks cycles and maintenance. This ensures compliance with regulations and patient safety. Clear records also facilitate quality control audits and accountability, maintaining operational efficiency and trust in sterile processing outcomes.
Sterilization Techniques and Methods
Explore primary sterilization methods like autoclaving, chemical sterilization, and radiation, ensuring the elimination of pathogens to maintain safety and quality in healthcare settings.
3.1 Autoclaving: Process and Parameters
Autoclaving uses high-pressure steam to sterilize instruments. Key parameters include temperatures (121°C or 134°C), pressure (15 psi), and exposure time (15-30 minutes). These settings ensure microbial elimination. Proper loading, packaging, and post-cycle cooling are critical for effectiveness. Autoclaving is widely used due to its reliability and compatibility with most medical materials, making it a cornerstone in sterile processing protocols. Adhering to these parameters guarantees safe and effective sterilization outcomes.
3.2 Chemical Sterilization: Types and Applications
Chemical sterilization involves using disinfectants like hydrogen peroxide, ozone, and glutaraldehyde to eliminate microbes. These methods are ideal for heat-sensitive equipment. Hydrogen peroxide is commonly used for its effectiveness and safety, while ozone offers rapid sterilization. Glutaraldehyde is versatile but requires longer exposure times. Proper ventilation and safety protocols are essential to avoid chemical hazards. These methods ensure sterilization of items unsuitable for autoclaving, maintaining their integrity and functionality.
3.3 Radiation and Filtration Methods
Radiation sterilization uses ionizing rays, such as gamma rays or X-rays, to kill microorganisms, ideal for heat-sensitive materials. Filtration methods, like HEPA filters, remove airborne pathogens, ensuring clean environments. Both techniques require strict safety protocols to prevent radiation exposure and maintain air quality. These methods are critical for sterilizing items that cannot withstand heat, ensuring patient safety and infection control in healthcare settings while minimizing contamination risks.

Infection Control and Safety Protocols
Adhering to strict infection control protocols ensures patient safety. Proper use of PPE, decontamination procedures, and waste management are critical to maintaining asepsis in sterile processing environments.
4.1 Personal Protective Equipment (PPE)
Wearing appropriate Personal Protective Equipment (PPE) is essential for preventing exposure to pathogens and maintaining asepsis. This includes gloves, gowns, masks, and eye protection. Proper donning and doffing techniques ensure safety and compliance with infection control standards. PPE selection varies based on task requirements and potential biohazard exposure. Adherence to guidelines from organizations like OSHA and CDC is critical for effective PPE use in sterile processing environments.
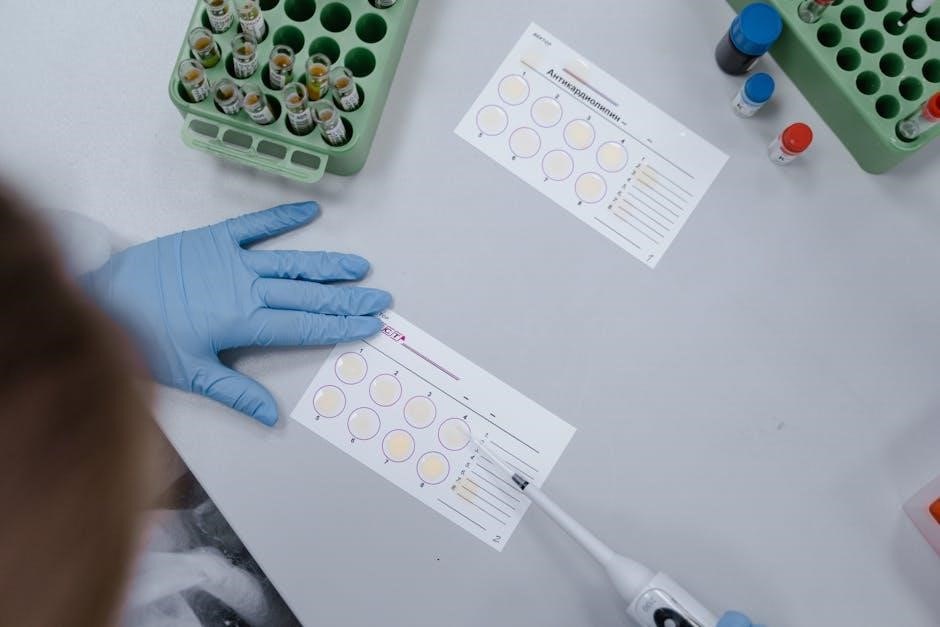
4.2 Decontamination and Cleaning Procedures
Effective decontamination and cleaning are critical to remove organic matter and contaminants from instruments. Methods include manual cleaning, ultrasonic cleaning, and enzymatic solutions. Proper cleaning ensures instruments are ready for sterilization and prevents cross-contamination. Strict adherence to standardized protocols is essential to maintain safety and efficiency in sterile processing environments. Improper cleaning can compromise sterilization effectiveness and patient safety, making it a cornerstone of infection control practices.
4.3 Biological Safety and Waste Management
Proper handling of infectious waste and biological materials is crucial to prevent contamination and exposure risks. Segregation of waste into biohazard containers ensures safe disposal. Autoclaving is commonly used to treat infectious waste before disposal. Adherence to biological safety protocols and regulatory guidelines is essential to maintain a safe environment for patients and staff, minimizing biohazard risks and ensuring compliance with infection control standards.
Quality Assurance and Regulatory Compliance
Adhering to strict standards ensures sterilization efficacy and patient safety. Accreditation agencies enforce compliance with regulations, while continuous quality control measures prevent contamination and maintain operational integrity.
5.1 Standards for Sterile Processing Departments
Sterile processing departments must adhere to rigorous standards to ensure patient safety and infection control. These standards, set by organizations like the Healthcare Sterile Processing Association (HSPA), encompass sterilization parameters, equipment maintenance, and staff training. Compliance with guidelines from the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) is critical to maintaining high-quality sterilization processes and preventing contamination risks.
5.2 Role of Accreditation Agencies
Accreditation agencies play a vital role in ensuring sterile processing departments meet standardized protocols. Organizations like the Healthcare Sterile Processing Association (HSPA) evaluate departments for compliance with industry standards, providing certifications that validate competency. These agencies also offer educational resources and guidelines to help departments maintain high levels of quality and safety, ensuring adherence to best practices in sterilization and infection control.
5.3 maintaining Quality Control Measures
5.3 Maintaining Quality Control Measures
Maintaining quality control measures ensures sterility and safety in sterile processing. This involves regular monitoring of sterilization cycles, biological and chemical testing, and proper documentation. Adhering to industry standards and protocols is crucial for consistency and reliability. Continuous improvement through staff training and process audits helps uphold high-quality outcomes, ensuring patient safety and compliance with regulatory requirements.

Certification Exam Preparation
Effective exam preparation involves targeted learning methods, including active recall, flashcards, and practice questions. Utilize AI-powered tools to streamline study materials and enhance retention for optimal results.
6.1 Certified Registered Central Service Technician (CRCST)
The Certified Registered Central Service Technician (CRCST) credential is essential for sterile processing professionals, validating expertise in infection control, sterilization, and quality assurance. Offered by the Healthcare Sterile Processing Association (HSPA), it ensures technicians meet high standards, preparing them for critical roles in healthcare settings. The certification covers key topics like decontamination, packaging, and sterilization methods, ensuring proficiency and compliance with industry regulations. Achieving CRCST enhances career opportunities and demonstrates commitment to patient safety and professional excellence.
6.2 Exam Content Outline and Format
The CRCST exam content outline includes key areas such as infection control, sterilization techniques, and quality assurance, ensuring a comprehensive assessment of sterile processing skills. The format typically involves multiple-choice questions, testing both theoretical knowledge and practical application. Understanding the exam structure and content is crucial for effective preparation, allowing candidates to focus on critical topics and improve their readiness for the certification process.
6.3 Strategies for Successful Exam Preparation
Effective exam preparation involves using AI-powered study tools, flashcards, and practice questions to reinforce key concepts. Active recall and targeted learning methods, such as focusing on weak areas, enhance retention. Regularly reviewing the exam content outline ensures alignment with test topics. Time management and consistent study schedules are crucial, while incorporating real-world case studies provides practical insights, helping candidates apply theoretical knowledge to real scenarios for better exam performance.
Tools and Resources for Effective Studying
This section explores essential tools for studying, including AI-powered study guide makers, flashcards, and practice questions, to enhance learning efficiency and improve exam preparation outcomes.
7.1 AI-Powered Study Guide Makers
AI-powered study guide makers simplify the creation of effective study materials by extracting key points from notes and organizing them into structured guides. Tools like Coral AI and Scribes enable users to transform PDFs, textbooks, and lecture notes into comprehensive study aids, such as mind maps and flashcards. These platforms also offer features like automated summarization, chat-enabled study materials, and practice exams, making exam preparation more efficient and tailored to individual needs for sterile processing technician certification.
7.2 Flashcards and Practice Questions
Flashcards and practice questions are essential tools for mastering sterile processing concepts. Platforms like PTCB Hero and AI-powered study guides offer tailored practice exams with detailed explanations, enhancing understanding. Active recall and spaced repetition techniques ensure long-term retention of critical information, making these resources invaluable for exam preparation and professional competency in sterile processing technician roles.
7.3 Utilizing the Sterile Processing Technical Manual
The Sterile Processing Technical Manual is a foundational resource for technicians, offering detailed insights into infection control, sterilization techniques, and quality assurance. It aligns closely with exam content, providing practical applications and case studies. This manual is essential for both new and experienced technicians, ensuring a comprehensive understanding of industry standards and best practices to excel in the field and achieve certification success.
Real-World Applications and Case Studies
Explore practical scenarios and real-world challenges in sterile processing, enhancing understanding through case studies that highlight teamwork, problem-solving, and adherence to infection control protocols effectively.
8.1 Case Studies in Sterile Processing
Case studies provide real-world examples of challenges faced in sterile processing, such as instrument contamination or sterilization failures. These scenarios highlight the importance of adherence to protocols, effective teamwork, and problem-solving. By analyzing these cases, technicians can learn best practices, understand common pitfalls, and improve their ability to handle complex situations. Practical insights from these studies enhance preparation for certification exams and real-world applications in healthcare settings.
8.2 Examples of Common Challenges and Solutions
Common challenges in sterile processing include instrument contamination, equipment malfunctions, and human error. Solutions involve strict adherence to protocols, regular maintenance of sterilization equipment, and ongoing staff training. Proper labeling and documentation also help mitigate errors. Addressing these challenges ensures patient safety, maintains efficiency, and upholds quality standards in healthcare facilities. Implementing these solutions is crucial for effective sterile processing operations and certification preparation.
8.3 The Role of Teamwork in Sterile Processing
Teamwork is essential in sterile processing, as it ensures efficient workflow, patient safety, and adherence to infection control protocols. Collaboration between technicians, surgical staff, and supervisors minimizes errors and enhances communication. Strong teamwork skills, including active participation and mutual respect, are vital for maintaining high standards and achieving departmental goals. Effective coordination ensures that sterile supplies are prepared and delivered safely and efficiently, supporting successful surgical outcomes.
Advances in Technology and Future Trends
Emerging technologies, such as AI and automated systems, are transforming sterile processing. These advancements enhance efficiency, reduce errors, and improve patient safety, shaping the future of the field.
9.1 Automated Instrument Processing Systems
Automated instrument processing systems streamline workflows, enhancing efficiency and consistency. These systems integrate advanced technologies, such as AI, to optimize sterilization cycles, reduce human error, and ensure compliance with safety standards. By automating key steps, these tools enable technicians to focus on critical tasks, improving overall productivity and patient care quality. Their adoption is revolutionizing sterile processing, offering scalable solutions for modern healthcare facilities.
9.2 Emerging Sterilization Technologies
Emerging sterilization technologies, such as hydrogen peroxide gas/plasma and ozone-based systems, offer enhanced efficiency and safety. These methods reduce chemical exposure and cycle times while maintaining effectiveness against resistant pathogens. Advanced technologies integrate real-time monitoring and data analytics, ensuring precise control and compliance with standards. Such innovations are transforming sterilization processes, providing eco-friendly and reliable solutions for modern healthcare settings and improving patient safety.
9.3 The Impact of AI on Sterile Processing
AI is revolutionizing sterile processing by enhancing efficiency and consistency. AI-powered tools optimize sterilization cycles, predict equipment maintenance needs, and ensure compliance with standards. Advanced algorithms analyze data to improve infection control and reduce errors. AI also aids in training through interactive simulations and personalized study guides, fostering better learning outcomes. These technologies are transforming the field, enabling safer and more reliable sterilization processes while supporting technician proficiency and patient safety.
